Distinguishing LDL types: Learn about pathogenic small-dense LDL and non-pathogenic large-buoyant LDL, and their role in arterial plaque. Manage plaque and maintain healthy arteries.
Introduction
Today, let’s explore the world of LDL types and how they contribute to arterial plaque. Plaque, composed of cholesterol, calcium, and protein, can accumulate in the arteries, leading to various health issues.
There are two types of plaque: soft plaque, which is unstable and dangerous, and hard plaque, which is calcified and less dangerous.
While the CAC test detects calcified plaque, it may not reflect soft plaque. The CAC paradox occurs when the CAC score rises after adopting a healthy lifestyle, indicating the conversion of soft plaque to hard plaque.
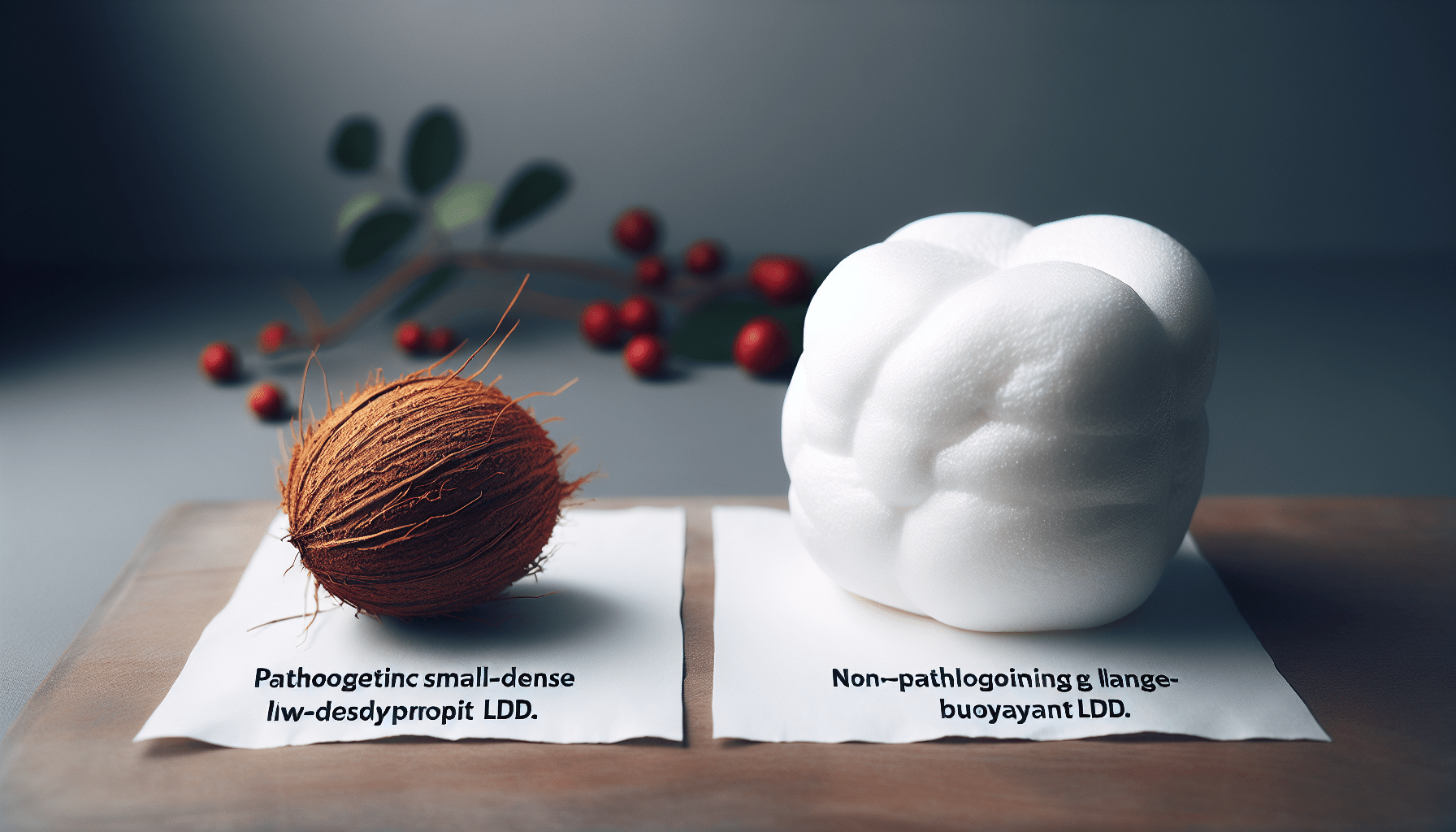
Understanding the distinction between pathogenic small-dense LDL and non-pathogenic large-buoyant LDL is crucial in managing arterial plaque.
Tests such as myeloperoxidase and Lp-PLA2, as well as ultrasounds, aid in detecting soft plaque. Furthermore, improving HDL levels and reducing triglycerides can be beneficial.
Natural nutrients like pycnogenol, gotu kola, vitamin K2, nattokinase, and niacin can help remove arterial plaque.
Additionally, tocotrienols, berberine, aged garlic, magnesium, potassium, and vitamin D play a role in naturally combating plaque buildup.
It’s essential to understand the role of different LDL types and the potential strategies for maintaining healthy arteries.
Understanding Plaque in the Arteries
Plaque in the arteries is composed of cholesterol, calcium, and protein. It acts as a band-aid, forming to protect the inside of the artery when inflammation or other issues occur.
There are two types of plaque: soft plaque and hard plaque. Soft plaque is unstable and more dangerous, while hard plaque is calcified, stable, and less dangerous.
Soft plaque is four times more common than calcified plaque, making it crucial to detect and address.

This image is a property of i.ytimg.com.
Composition of plaque
As mentioned earlier, plaque is made up of cholesterol, calcium, and protein. These three components combine to form a band-aid-like substance that serves as a protective barrier inside the artery.
Types of plaque: soft and hard
There are two types of plaque: soft plaque and hard plaque. Soft plaque is unstable and dangerous, while hard plaque is calcified, more stable, and less dangerous.
Soft plaque is four times as common as calcified plaque, making it a significant concern when it comes to cardiovascular health.
Importance of Distinguishing LDL Types
Understanding the different types of LDL (low-density lipoprotein), also known as “bad” cholesterol, is essential in determining the risk and formation of plaque in the arteries.
LDL plays a vital role in plaque formation, as it transports cholesterol to the artery walls. However, it is crucial to differentiate between small-dense and large-buoyant LDL to better assess the severity of plaque development.
Role of LDL in plaque formation
LDL plays a critical role in plaque formation, as it carries cholesterol to the artery walls. It can become oxidized and glycation can occur, which further contributes to the formation of plaque.
Differentiating between small-dense and large-buoyant LDL
There are two types of LDL: small-dense pathogenic LDL and large-buoyant non-pathogenic LDL. Small-dense LDL particles are more dangerous and associated with the formation of soft plaque.
On the other hand, large-buoyant LDL particles are relatively less harmful and do not contribute significantly to plaque formation.
Glycation and Oxidation of LDL
Glycation and oxidation play a significant role in the development of soft plaque. Glycation occurs when a sugar molecule attaches to a protein molecule, causing inflammation and other issues in the body. Additionally, LDL can become oxidized, further contributing to plaque formation.
These processes affect the structure and function of LDL, making it more likely to contribute to soft plaque formation.
Association of glycation and oxidation with soft plaque
Glycation and oxidation are closely associated with the formation of soft plaque. These processes can cause inflammation and damage to the artery walls, leading to the accumulation of plaque.
Effect on LDL structure and function
Glycation and oxidation modify the structure and function of LDL. These modifications make LDL more susceptible to contributing to plaque formation and increase the risk of cardiovascular issues.
Identifying Soft Plaque
Detecting soft plaque is crucial for accurately assessing the risk of cardiovascular issues.
Several indicators can help identify the presence of soft plaque in the arteries, including the role of myeloperoxidase (MPO) and Lp-PLA2, as well as certain blood tests.
However, it is essential to acknowledge the limitations of some detection methods, such as the CAC (coronary artery calcium) test.
Role of Myeloperoxidase and Lp-PLA2
Myeloperoxidase (MPO) and Lp-PLA2 are biomarkers that can indicate the presence of soft plaque in the arteries. High levels of these biomarkers may suggest a higher risk of soft plaque development.
Blood test indicators of soft plaque
Certain blood tests can provide insights into the presence of soft plaque in the arteries. Testing for Myeloperoxidase (MPO) and Lp-PLA2 can help assess the risk of soft plaque development.
Limitations of CAC test
The CAC test, while valuable in detecting calcified plaque, may not accurately reflect the presence or severity of soft plaque. This test primarily focuses on calcified plaque, potentially missing the early stages of plaque formation.
Ultrasound: Detecting Soft Plaque
Ultrasound imaging is an effective method to detect soft plaque in the arteries. It operates on the principles of sound waves and provides visualization of the arteries, including the presence of soft plaque.
While ultrasound has advantages in detecting soft plaque, it also has limitations.
Principles of ultrasound imaging
Ultrasound imaging utilizes high-frequency sound waves that bounce off the body’s tissues to create an image. By analyzing the reflected waves, healthcare professionals can visualize and assess the presence of soft plaque in the arteries.

Visualization of soft plaque
Ultrasound imaging allows healthcare professionals to visualize the presence of soft plaque in the arteries. This non-invasive method provides valuable information about plaque development and potential cardiovascular risks.
Advantages and limitations
Ultrasound imaging offers several advantages, such as its non-invasive nature and ability to detect soft plaque. However, it also has limitations, including the dependence on the expertise of the operator and the difficulty in assessing plaque severity accurately.
Optimal Lipid Profile for Plaque Reduction
Reaching an optimal lipid profile is crucial for reducing plaque formation in the arteries. Maintaining higher levels of HDL (high-density lipoprotein) while lowering triglycerides can have significant benefits in cleaning up bad LDL and reducing the risk of plaque development.
Importance of HDL levels
HDL, often known as “good” cholesterol, plays a vital role in cleaning up bad LDL and reducing the risk of plaque formation. Maintaining higher levels of HDL can help mitigate cardiovascular risks.
Role of triglycerides
High levels of triglycerides may suggest an excessive intake of carbohydrates. Lowering triglyceride levels is essential for reducing the risk of plaque formation and improving cardiovascular health.
Strategies to increase HDL and reduce triglycerides
Several strategies can help increase HDL levels and reduce triglycerides. These include adopting a healthy diet, engaging in regular physical activity, and considering certain medications or supplements under medical supervision.
Nutrients for Natural Plaque Removal
Certain nutrients have been found to aid in the natural removal of arterial plaque. By incorporating these nutrients into your diet, you can potentially support the reduction of plaque buildup and promote better cardiovascular health.

Pycnogenol: Benefits and Mechanisms of action
Pycnogenol, derived from pine bark, offers various benefits in reducing plaque formation. It helps convert soft plaque to calcified plaque, improves plaque stability, and prevents plaque formation.
Gotu Kola: Role in plaque reduction
Gotu Kola is an herb that has been traditionally used for its medicinal properties. It helps enhance the function of pycnogenol, leading to the conversion of soft plaque to more stable, calcified plaque.
Vitamin K2: Effects on calcium deposition in arteries
Vitamin K2 is a potent inhibitor of vascular calcification, meaning it can slow down the process of calcium deposition in the arteries. This can help prevent the formation of plaque and promote arterial health.
Nattokinase: Fibrinolytic properties and plaque reduction
Nattokinase is an enzyme derived from fermented soybeans. It possesses fibrinolytic properties, which means it helps dissolve fibrin, a protein involved in the formation of plaque.
By promoting fibrinolysis, nattokinase aids in plaque reduction.
Niacin: Effects on lipoprotein metabolism
Niacin, also known as vitamin B3, can have positive effects on lipoprotein metabolism. It can help improve the lipid profile by increasing HDL levels and reducing triglycerides, which in turn aids in plaque reduction.
Additional Nutrients for Plaque Reduction
Several other nutrients deserve recognition for their potential role in reducing plaque buildup in the arteries. These nutrients, including tocotrienols, berberine, aged garlic, magnesium, potassium, and vitamin D, offer various benefits for cardiovascular health and plaque reduction.
Tocotrienols: Antioxidant properties and arterial health
Tocotrienols, a form of vitamin E, possess antioxidant properties that contribute to arterial health. They help reduce inflammation, oxidative stress, and promote the removal of plaque from the arteries.
Berberine: Effects on lipid metabolism and inflammation
Berberine, a compound found in certain plants, has been shown to have beneficial effects on lipid metabolism and inflammation. It can help improve cholesterol levels, reduce inflammation, and potentially aid in plaque reduction.
Aged Garlic: Benefits for cardiovascular health
Aged garlic, a form of garlic that has undergone a fermentation process, offers numerous benefits for cardiovascular health. It helps lower cholesterol levels, reduces blood pressure, and may contribute to the removal of plaque from the arteries.
Magnesium: Role in vascular health
Magnesium plays a crucial role in vascular health. It helps relax the smooth muscles of the blood vessels, potentially reducing plaque buildup and improving overall cardiovascular function.
Potassium: Effects on blood pressure and arterial function
Potassium is an essential mineral that plays a role in maintaining healthy blood pressure and arterial function. By promoting proper blood flow and reducing the risk of hypertension, potassium supports arterial health and plaque reduction.
Vitamin D: Impacts on immune function and inflammation
Vitamin D, also known as the “sunshine vitamin,” is involved in various physiological processes, including immune function and inflammation.
Adequate levels of vitamin D help regulate these functions, potentially reducing the risk of plaque formation and improving cardiovascular health.
Conclusion
In conclusion, understanding plaque in the arteries and its composition is crucial for assessing cardiovascular health.
Distinguishing between LDL types, identifying soft plaque, and utilizing detection methods like ultrasound can aid in assessing plaque severity accurately.
Achieving an optimal lipid profile and incorporating specific nutrients into the diet can help reduce plaque formation naturally.
Further research in this field is warranted to explore additional strategies for plaque reduction and arterial health improvement.
By taking appropriate measures and adopting a holistic approach to cardiovascular health, we can work towards a healthier future with reduced plaque buildup and improved overall well-being.