Discover how fatty liver disease can impact life expectancy. Explore the potential implications, management strategies, and importance of early detection.
Did you know that having a fatty liver disease can significantly impact your life expectancy?
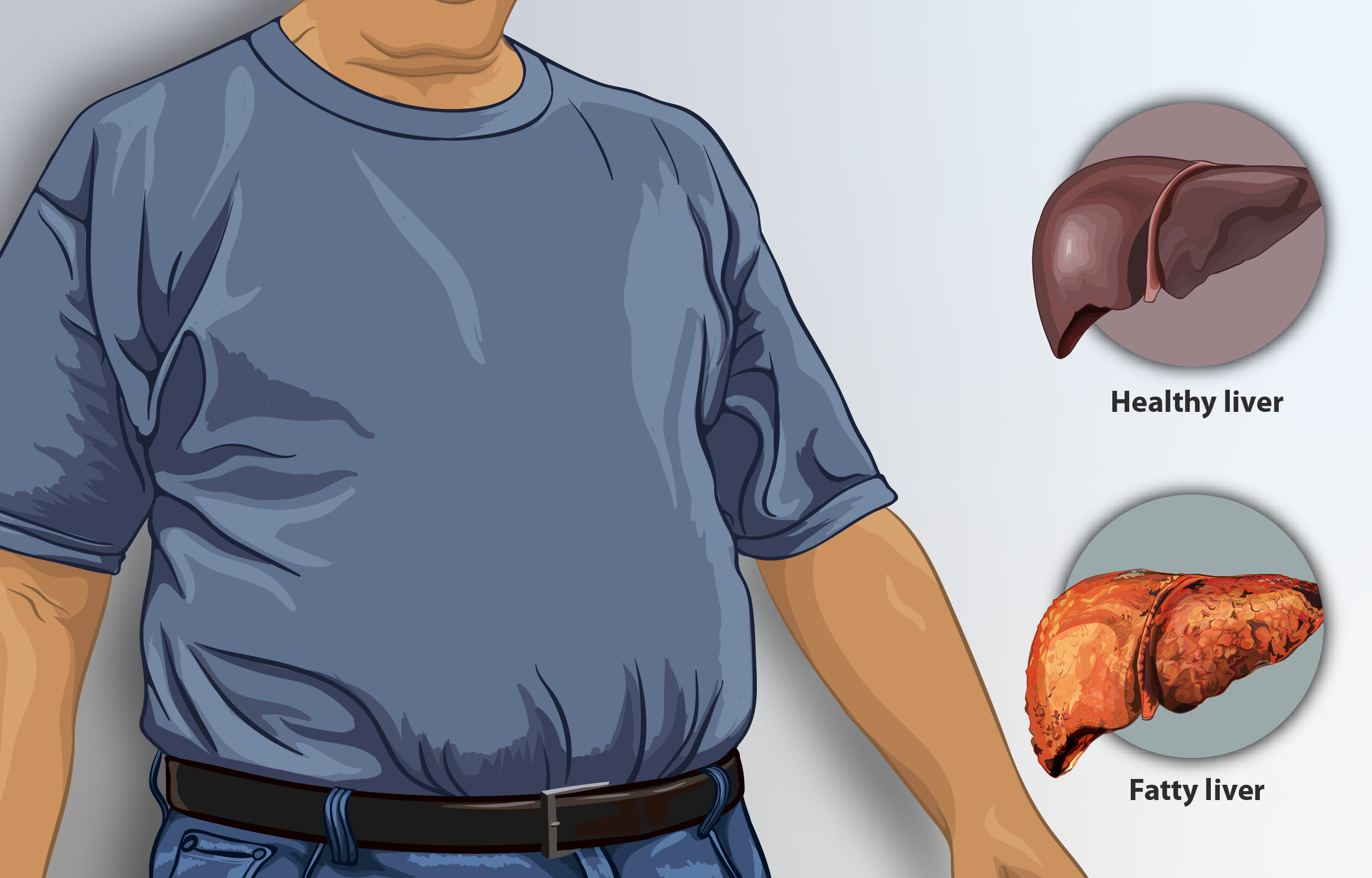
This condition, characterized by a buildup of fat in the liver, can lead to serious complications if left untreated.
In this article, we will explore the potential implications of fatty liver disease on your longevity and discuss ways to improve your overall prognosis.
So, if you or someone you know is living with this condition, read on to discover the importance of early detection and proactive management in extending a healthy and fulfilling life.

Overview of Fatty Liver Disease
Fatty liver disease, also known as hepatic steatosis, is a condition characterized by excessive fat accumulation in the liver.
It is a common health issue that affects millions of people worldwide. When the amount of fat in the liver exceeds 5–10% of its weight, it can lead to liver inflammation and damage.
Fatty liver disease can be categorized into two main types: alcoholic fatty liver disease (AFLD) and non-alcoholic fatty liver disease (NAFLD).
Definition of Fatty Liver Disease
Fatty liver disease is a medical condition in which there is an abnormal accumulation of fat in the liver cells.
This excess fat can interfere with the normal functioning of the liver and lead to inflammation and scarring.
Fatty liver disease can be further classified into alcoholic fatty liver disease (AFLD) and non-alcoholic fatty liver disease (NAFLD), depending on the underlying cause.
Causes of Fatty Liver Disease
The main cause of AFLD is excessive alcohol consumption. Consuming large amounts of alcohol over a prolonged period can lead to liver inflammation and the accumulation of fat in the liver.
On the other hand, NAFLD is associated with metabolic factors such as obesity, insulin resistance, high blood pressure, and high cholesterol levels.
These factors contribute to the development of fatty liver disease in individuals who do not consume excessive alcohol.
Types of Fatty Liver Disease
Fatty liver disease can be broadly classified into two types: alcoholic fatty liver disease (AFLD) and non-alcoholic fatty liver disease (NAFLD).
AFLD occurs as a result of excessive alcohol consumption, while NAFLD is mainly associated with obesity and metabolic syndrome.
NAFLD is further divided into non-alcoholic fatty liver (NAFL), which does not involve liver inflammation, and non-alcoholic steatohepatitis (NASH), which is characterized by liver inflammation and damage.
Prevalence of Fatty Liver Disease
Fatty liver disease is a global health concern, with its prevalence on the rise in recent years.
It is estimated that approximately 25% of adults worldwide are affected by NAFLD, making it the most common liver disorder in the Western world. AFLD is more prevalent in individuals who consume excessive alcohol regularly.
The increasing rates of obesity, diabetes, and metabolic syndrome have contributed to the rising prevalence of NAFLD.
Factors Influencing Life Expectancy
Several factors can influence the life expectancy of individuals with fatty liver disease.
The severity of the disease, underlying conditions, comorbidities, and individual response to treatment all play a significant role in determining life expectancy.
Severity of Fatty Liver Disease
The severity of fatty liver disease can have a direct impact on life expectancy. In the early stages, when the condition is mild, the prognosis is generally favorable.
However, as the disease progresses, the liver becomes more inflamed and scarred, leading to advanced fibrosis, or cirrhosis.
The more severe the liver damage, the higher the risk of complications and reduced life expectancy.
Underlying Conditions
Underlying conditions such as obesity, diabetes, and metabolic syndrome can significantly affect the progression and prognosis of fatty liver disease.
These conditions often go hand in hand with NAFLD and can worsen liver inflammation and damage.
Proper management and control of these underlying conditions are crucial for improving life expectancy in individuals with fatty liver disease.
Comorbidities
Comorbidities, such as cardiovascular disease and chronic kidney disease, can further impact life expectancy in individuals with fatty liver disease.
These conditions often occur alongside fatty liver disease and can increase the risk of complications and mortality.
Close monitoring and appropriate management of comorbidities are necessary to improve overall prognosis and life expectancy.
Individual Response to Treatment
Each individual’s response to treatment can vary, which can also influence life expectancy.
Some individuals may respond well to lifestyle modifications, dietary changes, and medications, leading to improved liver health and prognosis.
Others may require more intensive interventions, such as liver transplantation, to improve life expectancy.
Proper medical supervision and personalized treatment plans based on individual responses are crucial in achieving the best possible outcomes.
Long-term Effects on Life Expectancy
If left untreated or poorly managed, fatty liver disease can have serious long-term effects on life expectancy.
The progression of the disease can lead to complications such as cirrhosis, liver failure, an increased risk of hepatocellular carcinoma (liver cancer), and cardiovascular complications.
Progression to Cirrhosis
As fatty liver disease progresses, it can lead to the development of cirrhosis, a condition characterized by irreversible scarring and fibrosis of the liver.
Cirrhosis significantly affects liver function and can result in liver failure if not properly managed.
The presence of cirrhosis is associated with a decrease in life expectancy due to the increased risk of complications.
Liver Failure
Liver failure occurs when the liver is no longer able to function properly. It can be a result of the progression of fatty liver disease, particularly in advanced stages such as cirrhosis.
Liver failure is a life-threatening condition that requires immediate medical intervention, such as a liver transplant, to prolong life expectancy.
Risk of Hepatocellular Carcinoma
Individuals with fatty liver disease, especially those with advanced fibrosis or cirrhosis, are at an increased risk of developing hepatocellular carcinoma (HCC), the most common form of liver cancer.
The presence of HCC significantly reduces life expectancy and necessitates prompt diagnosis and treatment.
Cardiovascular Complications
Fatty liver disease is closely associated with metabolic syndrome and obesity, both of which are risk factors for cardiovascular disease.
Individuals with fatty liver disease are more susceptible to developing conditions such as hypertension, heart disease, and stroke, which can further reduce life expectancy.
Therefore, it is important to manage both liver health and cardiovascular health to improve overall prognosis.
Management of Fatty Liver Disease
The management of fatty liver disease focuses on lifestyle modifications, dietary changes, weight loss, regular exercise, and, in some cases, the use of medications and supplements to improve liver health and the overall prognosis.
Lifestyle Modifications
Making lifestyle modifications is crucial in managing fatty liver disease. It involves quitting alcohol consumption (in the case of AFLD), adopting a healthy diet, maintaining a healthy weight, and engaging in regular physical activity.
These changes can help reduce liver inflammation, promote weight loss, and improve liver function.
Dietary Changes
A balanced and nutritious diet is essential for managing fatty liver disease.
It often involves reducing the intake of saturated fats, refined sugars, and processed foods and increasing the consumption of fruits, vegetables, whole grains, and lean proteins.
Dietary changes can help control weight, reduce hepatic fat accumulation, and improve liver health.
Weight Loss
Weight loss plays a crucial role in managing and improving fatty liver disease.
Losing excess weight can reduce liver fat accumulation, decrease inflammation, and improve insulin sensitivity.
Gradual and sustainable weight loss achieved through a combination of diet and regular exercise is considered the most effective approach.
Exercise Regimen
Regular physical activity is beneficial for individuals with fatty liver disease.
Engaging in aerobic exercises, such as brisk walking or jogging, as well as resistance training, can help burn excess fat, improve insulin sensitivity, and strengthen overall cardiovascular health.
Including exercise as part of a daily routine can contribute to better liver function and overall prognosis.
Medications and Supplements
In some cases, medications and supplements may be prescribed to individuals with fatty liver disease, especially in advanced stages or when lifestyle modifications alone are not sufficient.
These may include medications to treat underlying conditions such as diabetes or hypertension, as well as supplements such as vitamin E or omega-3 fatty acids that have shown potential benefits for liver health.
Close medical supervision is necessary when using medications and supplements to ensure safety and efficacy.

Importance of Early Diagnosis and Treatment
Early diagnosis and prompt treatment of fatty liver disease are crucial in preventing disease progression, reducing complications, improving quality of life, and potentially increasing life expectancy.
Impact on Disease Progression
Early diagnosis allows for timely interventions and lifestyle modifications that can slow down or even reverse disease progression.
By identifying fatty liver disease at an early stage, individuals have a higher chance of making the necessary changes to prevent further liver damage and improve their overall prognosis.
Preventing Complications
Detecting fatty liver disease early on enables healthcare providers to closely monitor individuals and implement preventive measures to reduce the risk of complications such as cirrhosis, liver failure, and liver cancer.
Early intervention and appropriate management can significantly improve outcomes and increase life expectancy.
Improving Quality of Life
Early diagnosis and treatment of fatty liver disease can lead to better management of symptoms, improved liver function, and an overall enhanced quality of life.
Individuals who receive early intervention and adopt appropriate lifestyle changes are more likely to experience less pain, fatigue, and discomfort associated with liver disease, leading to a better quality of life.
Potential Life Expectancy Increase
By addressing fatty liver disease at its early stages, individuals have a higher chance of successfully managing the condition and reducing the risk of life-threatening complications.
Early diagnosis and treatment can potentially increase life expectancy by preventing disease progression, preserving liver function, and improving overall health.
Liver Transplantation as a Treatment Option
In cases of advanced fatty liver disease, particularly when it progresses to cirrhosis or liver failure, liver transplantation may be considered as a treatment option.
Liver transplantation involves surgically replacing the diseased liver with a healthy liver from a deceased or living donor.
Indications for Liver Transplantation
Liver transplantation may be indicated for individuals with end-stage liver disease due to fatty liver disease, where the liver is no longer able to function adequately.
This can include individuals with advanced cirrhosis, liver failure, or hepatocellular carcinoma that cannot be successfully treated by other means.
Evaluation Process for Transplantation
The evaluation process for liver transplantation involves a comprehensive assessment of an individual’s overall health, including liver function, physical condition, and suitability for surgery.
It includes various medical tests, consultations, and discussions with the transplant team to determine eligibility and the best course of action.
Post-Transplant Care
After liver transplantation, individuals require lifelong care to ensure the transplanted liver functions properly and to prevent complications.
This includes taking immunosuppressant medications to prevent rejection, regular follow-up appointments with the transplant team, adherence to a healthy lifestyle, and close monitoring of liver function.
Survival Rates and Life Expectancy Post-Transplantation
Liver transplantation can significantly improve life expectancy in individuals with end-stage liver disease due to fatty liver disease.
The survival rates post-transplantation have improved over the years, and the average life expectancy after a liver transplant is around 20 years or more.
However, individual factors, such as age, overall health, and the presence of comorbidities, can influence the long-term success of the transplant and life expectancy.
Prognosis for Different Stages of Fatty Liver Disease
The prognosis for individuals with fatty liver disease varies depending on the stage and severity of the disease.
Different stages, including non-alcoholic fatty liver disease (NAFLD), non-alcoholic steatohepatitis (NASH), advanced fibrosis, and cirrhosis, have different implications for life expectancy.
Non-Alcoholic Fatty Liver Disease (NAFLD)
In the early stages of NAFLD, individuals typically have a good prognosis, as the liver is still functioning relatively well.
With appropriate lifestyle modifications and disease management, it is possible to reverse or halt the progression of the disease and improve life expectancy.
Non-Alcoholic Steatohepatitis (NASH)
NASH is a more advanced stage of fatty liver disease that involves liver inflammation and damage.
The prognosis for individuals with NASH is generally less favorable, as there is an increased risk of disease progression and the development of complications such as cirrhosis or liver cancer.
However, with early diagnosis, lifestyle changes, and proper medical management, the prognosis can be improved.
Advanced Fibrosis
Advanced fibrosis refers to significant scarring and damage to the liver, often a result of untreated or uncontrolled fatty liver disease.
At this stage, the prognosis can be more concerning, as there is an increased risk of developing cirrhosis or liver failure.
Close monitoring, appropriate interventions, and adherence to treatment plans are crucial to slow down disease progression and preventing further liver damage.
Cirrhosis
Cirrhosis is the most advanced stage of fatty liver disease, marked by extensive liver scarring and impaired liver function.
The prognosis for individuals with cirrhosis is generally poor, as there is an increased risk of complications such as liver failure or hepatocellular carcinoma.
Liver transplantation may be the only viable option for improving life expectancy at this stage.
Risk Factors that Impact Life Expectancy
Several risk factors can impact the life expectancy of individuals with fatty liver disease.
These risk factors, including obesity, type 2 diabetes, metabolic syndrome, alcohol consumption, and hepatitis C coinfection, can worsen liver inflammation, increase liver damage, and lead to complications.
Obesity
Obesity is closely associated with the development and progression of fatty liver disease.
Excess body weight, particularly abdominal adiposity, contributes to liver fat accumulation and inflammation.
Obesity increases the risk of advanced liver disease and reduces the life expectancy in individuals with fatty liver disease.
Type 2 Diabetes
Type 2 diabetes is a significant risk factor for non-alcoholic fatty liver disease (NAFLD). Insulin resistance and elevated blood sugar levels contribute to liver inflammation and fat accumulation.
Individuals with both fatty liver disease and type 2 diabetes often experience more severe liver damage and have a poorer prognosis compared to those without diabetes.
Metabolic Syndrome
Metabolic syndrome is a cluster of conditions, including obesity, high blood pressure, high blood sugar, and abnormal cholesterol levels.
It significantly increases the risk of developing fatty liver disease and can worsen the prognosis.
Individuals with fatty liver disease and metabolic syndrome are more likely to experience disease progression and complications.
Alcohol Consumption
Excessive alcohol consumption is a key risk factor for alcoholic fatty liver disease (AFLD).
Regular and heavy alcohol intake can lead to liver inflammation, fat accumulation, and liver damage.
Alcohol can exacerbate the progression of fatty liver disease and decrease life expectancy in affected individuals.
Hepatitis C Coinfection
Individuals with fatty liver disease who are also coinfected with hepatitis C virus (HCV) face a more challenging prognosis.
Hepatitis C infection can worsen liver inflammation, lead to fibrosis or cirrhosis, and increase the risk of liver cancer.
The combination of fatty liver disease and hepatitis C coinfection significantly impacts life expectancy and necessitates appropriate medical management.
Effects of Lifestyle Changes on Life Expectancy
Making lifestyle changes can have a profound impact on the life expectancy of individuals with fatty liver disease.
Addressing modifiable risk factors, such as diet, physical activity, smoking, and alcohol consumption, can lead to improved liver health and overall prognosis.
Role of Diet and Nutrition
Adopting a healthy diet is crucial for individuals with fatty liver disease.
Consuming a balanced diet rich in fruits, vegetables, whole grains, and lean proteins while minimizing the intake of saturated fats, refined sugars, and processed foods can help reduce liver fat accumulation and inflammation, improve insulin sensitivity, and promote a healthier liver.
Physical Activity and Exercise
Regular physical activity and exercise play a vital role in managing fatty liver disease.
Engaging in aerobic exercises, such as walking, jogging, or swimming, as well as resistance training, can help burn excess fat, improve insulin sensitivity, and reduce inflammation.
Incorporating regular exercise into daily routines can contribute to better liver function and increase life expectancy.
Smoking Cessation
Smoking has detrimental effects on liver health and can worsen the progression of fatty liver disease.
Quitting smoking is essential for improving liver function, reducing inflammation, and decreasing the risk of complications.
Smoking cessation can significantly contribute to a better prognosis and longer life expectancy for individuals with fatty liver disease.
Alcohol Abstinence
For individuals with alcoholic fatty liver disease (AFLD), complete alcohol abstinence is crucial to managing the condition and improving life expectancy.
Eliminating alcohol consumption can halt disease progression, reduce liver inflammation, and improve liver function.
It is essential to seek support from healthcare professionals or support groups to successfully abstain from alcohol.
Research and Future Perspectives
Research on fatty liver disease is ongoing, aiming to better understand the condition, identify new therapeutic targets, and develop more effective strategies for diagnosis, prevention, and treatment.
Several areas of research and future perspectives have emerged in recent years.
Current Studies on Fatty Liver Disease
Numerous studies are currently being conducted to investigate various aspects of fatty liver disease, including its underlying mechanisms, risk factors, progression, and potential treatment options.
Research focuses on understanding the impact of lifestyle interventions, medications, and targeted therapies on liver health and overall prognosis.
Potential Therapies and Treatments
Researchers are exploring various potential therapies and treatments for fatty liver disease.
This includes the development of medications and interventions to reduce liver fat accumulation, inflammation, and fibrosis.
Targeted therapies that aim to improve insulin sensitivity, regulate lipid metabolism, and reduce oxidative stress show promising results in preclinical and clinical studies.
Improved Diagnostic Methods
Efforts are being made to develop non-invasive diagnostic methods for fatty liver disease.
Non-invasive imaging techniques, such as transient elastography and magnetic resonance imaging (MRI), are being used to assess liver stiffness and fat content.
These methods can provide valuable information about liver health, aid in disease staging, and guide treatment decisions.
Preventive Strategies
Preventing fatty liver disease and its progression is a key area of focus for researchers.
Studies aim to identify early markers and risk factors for the development of fatty liver disease, allowing for targeted preventive strategies.
Lifestyle modifications, such as healthy eating and regular exercise, are also being explored as preventive measures to reduce the incidence and severity of fatty liver disease.
Conclusion
Fatty liver disease is a prevalent condition that can have significant implications for life expectancy if left untreated or poorly managed.
The severity of the disease, underlying conditions, comorbidities, and individual response to treatment all play a crucial role in determining prognosis and overall life expectancy.
Early diagnosis and prompt treatment, combined with lifestyle modifications, dietary changes, and appropriate medical interventions, are essential in improving liver health, preventing complications, and potentially increasing life expectancy.
Ongoing research and future perspectives offer hope for better understanding, improved diagnostic methods, and more effective therapeutic options for individuals with fatty liver disease.
By addressing modifiable risk factors and making positive lifestyle changes, individuals can take control of their liver health and improve their overall prognosis.